Food sensitivities can cause gut inflammation by triggering delayed immune responses, unlike food allergies which cause immediate reactions. This inflammation often leads to symptoms like bloating, gas, or irregular bowel movements and can contribute to conditions like autoimmune disorders. Identifying and managing food sensitivities requires understanding the difference between sensitivities (immune-related) and intolerances (non-immune digestive issues), tracking symptoms, and adjusting diet and lifestyle to reduce inflammation.
Key points:
- Food sensitivities involve immune responses, often delayed, causing inflammation.
- Food intolerances stem from digestive issues, like enzyme deficiencies (e.g., lactose intolerance).
- Chronic inflammation from sensitivities can affect mental and physical health.
- Gut bacteria imbalances (dysbiosis) can worsen sensitivities and inflammation.
- Steps to manage sensitivities include food journaling, elimination diets, and focusing on anti-inflammatory foods.
Addressing food sensitivities with professional guidance can improve gut health, reduce inflammation, and enhance overall well-being.
Food Sensitivities and Gut Integrity
Food Sensitivities vs. Food Intolerances: What’s the Difference
Food sensitivities and food intolerances may both lead to discomfort after eating certain foods, but they result from entirely different processes. Understanding these differences is key to finding the right treatment and management strategies.
The main distinction? Whether or not the immune system is involved. Sheila E. Crowe explains:
"The difference between a food allergy and a food intolerance is its immune basis."
This same principle applies when comparing food sensitivities to food intolerances. Sensitivities involve the immune system, while intolerances stem from digestive issues.
What Are Food Sensitivities?
Food sensitivities occur when the immune system mistakenly identifies certain foods as harmful, triggering an immune response. As ESNM Gut Microbiota for Health puts it:
"Sensitivities result from an inappropriate activation of the immune system upon exposure to a particular food."
Unlike food allergies, which involve IgE antibodies and cause immediate reactions, food sensitivities typically involve IgG antibodies and produce delayed responses. This delay can make it challenging to pinpoint the specific trigger. The immune response often releases inflammatory compounds, which can damage the gut lining over time. Latitude Food Allergy Care emphasizes the distinction:
"The crucial difference between a food sensitivity and a food allergy is that food allergies can be life-threatening and those with a food allergy must carry two epinephrine autoinjectors (such as an EpiPen®) at all times."
What Are Food Intolerances?
Food intolerances, on the other hand, are not immune-related. Instead, they occur when the body struggles to digest certain foods. ESNM Gut Microbiota for Health defines them as:
"An abnormal, non-immune mediated, functional response to a food."
Most food intolerances arise from a lack of specific enzymes needed to break down certain compounds. A well-known example is lactose intolerance, which affects about 65% of the global population after infancy. People with this condition lack enough lactase, the enzyme that digests lactose. As a result, undigested lactose ferments in the large intestine, causing symptoms like gas, bloating, cramping, and diarrhea.
UChicago Medicine explains:
"With food intolerances, the vast majority are not related to the immune system… An allergy or gastroenterology specialist can help you distinguish between a food allergy and an intolerance."
Other examples include histamine intolerance, which affects around 1% of the population, and other enzyme deficiencies. These conditions require different management strategies compared to sensitivities.
How Common Are Food Sensitivities and Their Effects on Gut Health?
Food sensitivities are more common than many realize. Research shows that about 20% of people worldwide experience adverse reactions to certain foods. Non-celiac wheat sensitivity (NCWS) is one example, with prevalence rates ranging from 0.6% to 6.0% in Western populations – and even up to 13% when based on self-reported symptoms.
Repeated immune responses to trigger foods can cause ongoing inflammation in the digestive tract. This highlights the importance of distinguishing between sensitivities and intolerances, as each requires a unique approach. While food intolerances might be managed with enzyme supplements or portion control, food sensitivities often call for eliminating trigger foods and supporting the immune system.
At Kinnection Clinic, a functional medicine approach helps identify whether symptoms stem from immune-mediated sensitivities or non-immune intolerances. Comprehensive testing and evaluations guide personalized treatment plans that address the root causes of digestive issues. Next, we’ll dive into how immune responses and gut imbalances contribute to inflammation.
How Food Sensitivities Cause Gut Inflammation
Food sensitivities can set off an immune system reaction that mistakenly targets harmless food proteins, causing inflammation that harms the gut lining. This process involves several immune mechanisms working together, leading to a cascade of inflammatory responses.
Immune System Overreaction
Food sensitivities arise when the immune system misidentifies certain food proteins as threats. Unlike the immediate reactions seen in food allergies, sensitivities trigger a slower, prolonged inflammatory response that can last for hours or even days after consuming the offending food.
As these trigger foods pass through the digestive system, immune cells release cytokines – chemical messengers that summon more immune cells to the area. This amplifies inflammation across the gut lining. At the same time, mediators like histamine increase blood vessel permeability, causing swelling in the tissues. Over time, this overreaction can spread throughout the digestive tract, leading to systemic inflammation and impairing the gut’s ability to recover.
The Role of Mast Cells and T-Cells in Inflammation
Certain immune cells, such as mast cells and T-cells, play a key role in escalating the inflammatory response. Mast cells, which are scattered throughout the gut lining, release inflammatory substances like histamine and leukotrienes when they encounter trigger foods.
Helper T-cells further intensify the response by releasing cytokines that attract additional immune cells to the site of inflammation. In some cases, these T-cells remain active for extended periods, contributing to chronic, low-grade inflammation that persists even between meals. Environmental factors, such as harmful gut bacteria, can worsen the situation by pushing the immune system into a more aggressive and inflammatory state, turning a normal interaction with food into an ongoing conflict.
Loss of Oral Tolerance
Oral tolerance refers to the immune system’s ability to recognize and accept food proteins without reacting. When this tolerance breaks down, the immune system becomes unbalanced, perceiving harmless foods as threats and triggering inflammation.
This breakdown can lead to various issues, such as IgE-mediated food allergies, celiac disease, and even increased vulnerability to infections. In some cases, the immune system may begin attacking the body’s own tissues, potentially leading to autoimmune disorders. Persistent gut inflammation further disrupts immune regulation, creating a cycle where inflammation perpetuates the loss of tolerance.
Rebuilding immune balance is crucial. At Kinnection Clinic, functional medicine approaches aim to address these disruptions by restoring oral tolerance. These strategies include promoting beneficial gut bacteria through whole foods, managing stress levels, and exploring targeted immune support, such as supplements or hormone balancing, when necessary. The goal is to reduce inflammation and help the digestive system regain its equilibrium.
sbb-itb-d9e542d
How Gut Bacteria Affect Food Sensitivities and Inflammation
The trillions of bacteria living in your gut play a major role in how your body reacts to the food you eat. When these microbial communities fall out of balance – a condition called dysbiosis – it can disrupt your immune system’s tolerance to food and lead to gut inflammation.
Gut Bacteria and Immune Tolerance
A well-balanced and diverse gut microbiome is essential for maintaining oral tolerance – your immune system’s ability to recognize food proteins as harmless. Beneficial bacteria in your gut help support regulatory T-cells (Tregs), which act as "peacekeepers" by preventing your immune system from overreacting.
"Under steady state, the intestinal microbiota has an essential role in maintaining a tolerogenic gut environment that prevents an inflammatory response against foreign antigens, mainly by promoting epithelial integrity and tolerogenic regulatory T (Treg) cell function".
Studies have found that children with food allergies often have lower microbial diversity and an altered bacterial balance compared to their healthy peers. This suggests that early imbalances in gut bacteria may increase the likelihood of developing food sensitivities. When the microbiome is disrupted, harmful bacteria and their toxins can trigger a stronger inflammatory response.
How Bacterial Imbalance Worsens Inflammation
Dysbiosis not only aggravates food sensitivities but can also lead to chronic inflammation. When harmful bacteria dominate, they may produce toxins that damage the gut lining, allowing food particles to "leak" into the bloodstream. This phenomenon, often referred to as "leaky gut", can provoke immune reactions.
"Food sensitivities are growing at a faster rate than genetic changes and the gut microbiota is one of the contributing factors".
Some bacterial strains can even alter how toxic certain food components are. For instance, certain bacteria may either increase or decrease the harmful effects of gluten, which explains why people with similar sensitivities sometimes experience different symptoms.
Bacterial Metabolites and Gut Health
Gut bacteria produce substances called metabolites that play a role in controlling inflammation. One key group of metabolites, short-chain fatty acids (SCFAs) like butyrate, helps regulate T-cell function and supports immune tolerance. When beneficial bacteria decline, the production of SCFAs drops, weakening this protective mechanism and making food sensitivities more likely.
On the flip side, some bacteria produce compounds like histamine, which can promote inflammation, or tryptophan derivatives that help shift immune responses toward a more anti-inflammatory state. If these beneficial bacteria are depleted, your gut loses an important line of defense against inflammation triggered by food.
"Dietary patterns constitute an important determinant of gut microbiota diversity, altering microbial community structure and metabolite production".
The encouraging news? You can influence the production of these protective metabolites through your diet. Eating fiber-rich foods, vegetables, and fermented products provides the nutrients that beneficial bacteria need to thrive. Clinics like Kinnection Clinic use targeted dietary strategies and probiotics to help restore a healthy bacterial balance and reduce inflammation.
How to Find and Manage Food Sensitivities
Figuring out and managing food sensitivities takes a thoughtful and step-by-step approach. By combining careful tracking, testing, and adjustments to your diet and lifestyle, you can identify problem foods and improve your gut health.
Steps to Find Food Sensitivities
The first step in identifying food sensitivities is to track what you eat and how your body responds. A food and symptom journal can be incredibly helpful:
"Generally, the best tool we have in identifying triggers with intolerances and sensitivities is a food symptom journal".
Write down everything you eat and note any symptoms, such as bloating, headaches, or fatigue. Over time, patterns may emerge – like dairy consistently causing discomfort or gluten leading to fatigue the next day.
Elimination diets are another powerful tool but should always be done under professional guidance:
"Trying to avoid multiple different foods can cause nutritional deficiency, so you don’t want to do an elimination diet on your own".
This process involves cutting out suspected trigger foods for 2–4 weeks and then reintroducing them one by one to observe your symptoms. It’s a systematic way to pinpoint specific sensitivities.
Specialized testing can provide additional clarity. For instance, hydrogen breath tests can reveal sensitivities to FODMAPs or conditions like SIBO. However, be cautious with at-home IgG antibody tests. The American Academy of Allergy, Asthma & Immunology advises against using these tests for diagnosing food sensitivities. Mayo Clinic nutritionists Krista Kerlinske and Lindsey Sefried caution:
"Food sensitivity or intolerance testing can lead to unnecessary food restrictions, increased stress and anxiety surrounding food, fear of foods, as well as overall poor nutrition and wellness".
Identifying your trigger foods is just the first step. The next move is adopting changes that reduce inflammation and promote gut health.
Diet and Lifestyle Changes
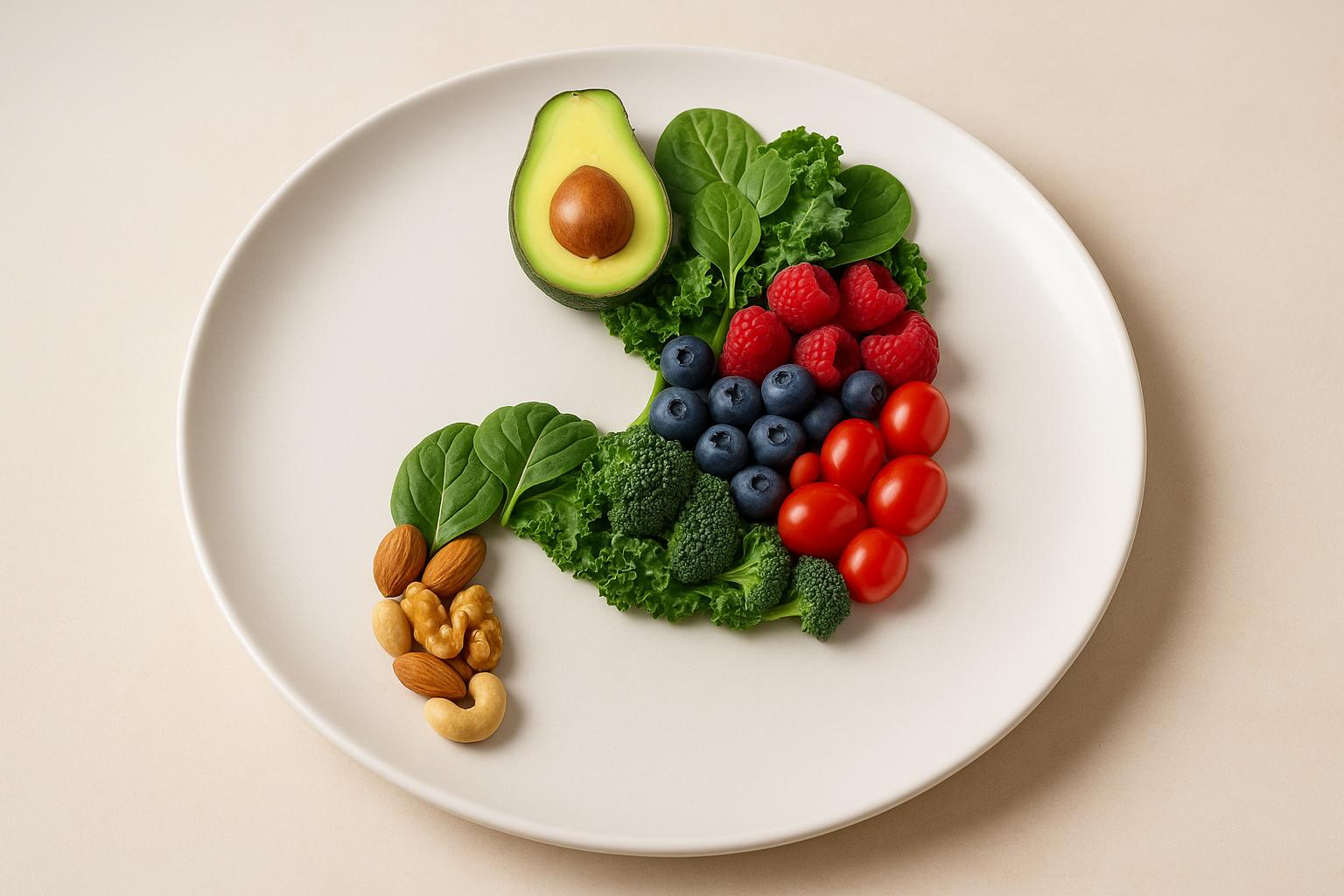
Once you’ve identified your triggers, managing sensitivities goes beyond avoiding certain foods. An anti-inflammatory diet can help soothe your gut. The Mediterranean diet, known for its omega-3 fatty acids, vitamin C, and polyphenols, is a great option for reducing inflammation.
Incorporate gut-friendly foods that support healthy bacteria and a strong intestinal lining. These include fiber-rich vegetables, fermented foods like kefir and sauerkraut, and omega-3–rich fish. Most Americans only consume about half the recommended daily fiber intake, so gradually increasing vegetables and whole grains can make a noticeable difference.
Lifestyle habits also play a big role. Poor sleep, chronic stress, and lack of exercise can all contribute to gut inflammation. Aim for 7–8 hours of sleep each night and 150–300 minutes of moderate exercise per week. Managing stress – whether through meditation, therapy, or simply talking about your feelings – can also help reduce inflammation.
Here are some simple food swaps to make your diet more gut-friendly:
| Instead of… | Try: |
|---|---|
| Charcuterie boards | Veggie slices with hummus |
| French fries | Baked sweet potatoes |
| Butter or cheese-based sauces | Olive oil, vinegar, and herbs |
| Grilled burgers | Grilled eggplant or portobello mushrooms |
| Cakes and pies | Dark chocolate with raspberries or grilled peaches |
As one nutrition expert puts it:
"To make any significant difference, it’s necessary to focus on long-term eating habits and an anti-inflammatory lifestyle".
For those dealing with multiple or complex sensitivities, a personalized approach can fine-tune these strategies.
Personalized Care for Long-Term Gut Health
Taking care of food sensitivities isn’t just about avoiding triggers – it’s about addressing the root causes of inflammation. Personalized care, such as functional medicine, focuses on understanding your unique health history and triggers.
At Kinnection Clinic, for example, practitioners use a combination of functional medicine principles and specialized testing to create tailored wellness plans. These plans may include nutritional support, gut microbiome testing, and other strategies to promote long-term gut health.
Professional guidance is especially important for those with multiple sensitivities or more complicated symptoms. A skilled practitioner can guide you through an elimination diet, interpret test results accurately, and develop sustainable management strategies. They can also help uncover other issues, like SIBO, that might be contributing to your food reactions.
The ultimate goal isn’t to restrict your diet forever but to heal your gut so you can enjoy a more varied diet over time.
Regular monitoring is crucial. As your gut heals and your needs evolve, check-ins with your healthcare provider and ongoing symptom tracking will help ensure your approach stays effective. While some improvements might be noticeable within weeks, fully restoring gut health and balance often takes months – or even years.
Conclusion: Steps to Better Gut Health
Taking control of your gut health starts with understanding the connection between food sensitivities, inflammation, and overall well-being. As highlighted earlier, recognizing how your immune system and microbiome interact allows you to take meaningful steps toward better health. Addressing food sensitivities early can help you avoid chronic inflammation, digestive issues, and even conditions like autoimmune disorders and other inflammatory diseases.
Improving gut health doesn’t have to feel overwhelming. Begin with simple, actionable steps: keep a food and symptom journal, prioritize whole, unprocessed foods, and collaborate with healthcare professionals who focus on identifying and addressing the root causes of inflammation. These foundational changes align with the broader discussion of immune responses and microbiome balance.
Small lifestyle adjustments today can lead to long-term benefits. Research underscores this: at age 50, men who adopted four or five low-risk lifestyle habits – such as avoiding smoking, maintaining a healthy BMI, staying active for at least 30 minutes daily, drinking alcohol in moderation, and eating a nutrient-rich diet – lived an average of 31.1 years free from chronic diseases. In contrast, those who adopted none of these habits lived just 23.5 years free of such conditions. For women, the difference was even more striking: 34.4 years versus 23.7 years.
Personalized care plays a crucial role in achieving lasting results. Studies show that a strong, empathetic relationship between patients and healthcare providers significantly improves outcomes in areas like weight management, quitting smoking, and increasing physical activity. At Kinnection Clinic, this personalized approach blends functional medicine principles with consistent support to help you identify triggers, implement sustainable changes, and track your progress. The goal isn’t just to alleviate symptoms – it’s to restore gut health so you can experience better energy, improved mood, and overall vitality.
Healing takes time and dedication. Managing food sensitivities and reducing inflammation can lead to noticeable improvements in mental clarity, mood, energy levels, and your overall quality of life.
Now is the time to act. Whether it’s starting a food journal, scheduling in-depth testing, or eliminating a single suspected trigger food, every small step brings you closer to a healthier gut and a better you.
FAQs
What’s the difference between food sensitivities and food intolerances?
Food sensitivities and food intolerances can trigger similar symptoms, but they affect the body in different ways. Food sensitivities are often tied to an immune system reaction, with symptoms that might show up hours or even days later. These can include headaches, fatigue, skin problems, or joint pain. On the other hand, food intolerances are usually related to the digestive system. They occur when the body struggles to break down certain foods due to a lack of specific enzymes, leading to immediate issues like bloating, gas, or diarrhea.
Pinpointing food sensitivities often involves elimination diets or food challenge tests, while identifying intolerances may require enzyme testing or simply paying close attention to how your body reacts to particular foods. Knowing the difference between the two can help you make smarter dietary choices and take better care of your gut health.
What dietary changes can help reduce gut inflammation from food sensitivities?
Managing gut inflammation linked to food sensitivities begins with an anti-inflammatory diet. Focus on eating whole, unprocessed foods like fresh fruits, vegetables, lean proteins, and healthy fats, such as olive oil and omega-3-rich fish. These choices can help soothe inflammation and improve gut health.
Equally important is identifying and steering clear of specific food triggers, which often include gluten, dairy, and heavily processed foods. Incorporating anti-inflammatory staples like leafy greens, tomatoes, nuts, and seeds can further enhance your gut health. By adjusting your diet to suit your body’s specific needs, you can take meaningful steps toward reducing inflammation and supporting overall wellness.
How does gut bacteria affect food sensitivities and inflammation?
The balance of gut bacteria is a major factor in how our bodies handle food sensitivities and inflammation. When the gut microbiome becomes unbalanced – a condition called dysbiosis – it can compromise the intestinal barrier. This can set off immune responses, leading to inflammation and making you more sensitive to certain foods.
On the flip side, a thriving gut microbiome, full of beneficial bacteria, plays a big role in keeping the immune system in check, calming inflammation, and potentially reducing food sensitivities. Taking care of your gut through a nutritious diet, incorporating probiotics, and managing stress can go a long way in supporting your overall health.