Adrenal fatigue is often discussed in functional medicine as a condition linked to stress disrupting cortisol production. While not officially recognized by major medical organizations, it’s described as Hypothalamic-Pituitary-Adrenal (HPA) axis dysregulation. Symptoms like fatigue, salt cravings, brain fog, and sleep issues are common. Accurate diagnosis is key to distinguishing adrenal fatigue from more severe conditions like Addison’s disease or Cushing’s syndrome.
Testing options include:
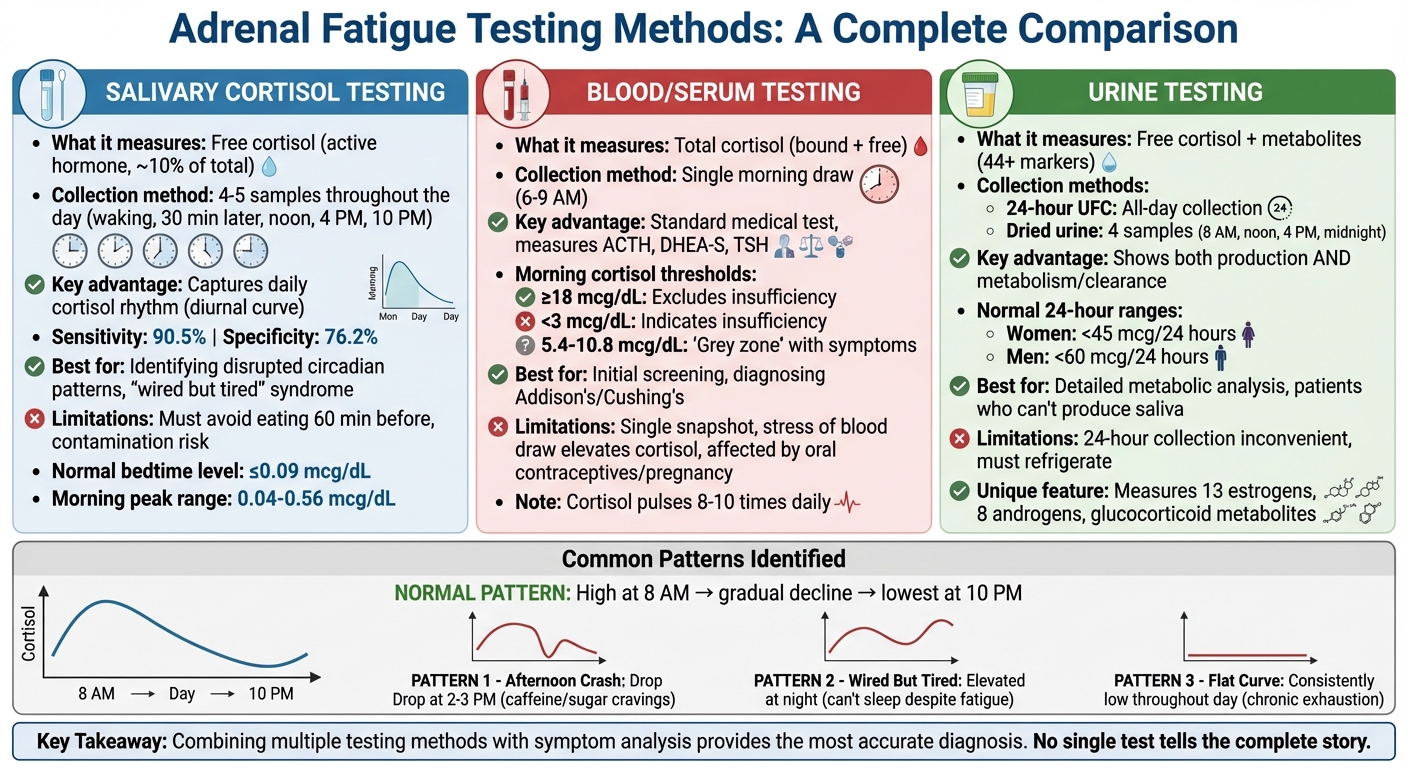
- Salivary Cortisol Testing: Tracks cortisol levels throughout the day, offering insight into daily hormone patterns.
- Blood Tests: Measures total cortisol and related hormones like ACTH, DHEA-S, and TSH for adrenal and thyroid function.
- Urine Testing: Evaluates cortisol metabolism over 24 hours or through multi-point dried urine samples.
Each method has strengths and limitations, but combining tests with symptom analysis provides clearer insights. Functional medicine practitioners often use these results to guide personalized care plans, focusing on reducing stress, improving sleep, and supporting adrenal health.
Adrenal Fatigue Testing Methods Comparison: Saliva, Blood, and Urine Tests
Salivary Cortisol Testing
How Salivary Cortisol Testing Works
Tracking cortisol levels throughout the day is essential for understanding HPA axis imbalances. Salivary cortisol testing provides a detailed view of these fluctuations by creating a diurnal curve. Unlike a single blood test that captures cortisol at just one moment, this method involves collecting saliva samples at multiple points during the day – typically upon waking, 30 minutes later, around noon, late afternoon (around 4:00 PM), and before bedtime (around 10:00 PM).
The process is simple. A specialized swab is placed in your mouth for 2–3 minutes until it’s fully saturated. Each sample is then labeled with the exact time of collection. To ensure accuracy, specific guidelines must be followed: avoid eating for at least 60 minutes before sampling, rinse your mouth with water 10 minutes prior, and refrain from brushing or flossing before collection to prevent contamination. Once collected, the samples should be refrigerated until they’re ready to be sent to the lab.
What makes salivary testing unique is that it measures only free cortisol – the active form of the hormone – which accounts for about 10% of your total cortisol. The other 90% is bound to proteins like albumin and cortisol-binding globulin (CBG). Blood tests, on the other hand, measure both bound and free cortisol together, which can sometimes lead to misleading results. This distinction is particularly important for pregnant women or those taking oral contraceptives, as these conditions can significantly increase protein-bound cortisol – sometimes by as much as 1.5 times. By focusing on free cortisol and capturing its daily rhythm, salivary testing provides a more detailed perspective on adrenal health.
Benefits and Limitations
Salivary cortisol testing is especially effective at identifying disrupted circadian rhythms that might be overlooked with single-point blood tests. For instance, it can reveal patterns like being "wired but tired", where cortisol remains elevated at bedtime instead of dropping to ≤0.09 mcg/dL. It can also detect a missing morning cortisol peak, which typically falls between 0.04 and 0.56 mcg/dL. Clinically, salivary cortisol shows a strong correlation (0.79) with free serum cortisol levels. When used alongside stimulation tests, it has demonstrated a sensitivity of 90.5% and a specificity of 76.2% for diagnosing adrenal insufficiency. Additionally, because samples are collected during normal daily activities, the stress-related spikes often caused by blood draws are minimized.
However, the test isn’t without its challenges. Saliva samples must be clear and uncontaminated – any issues may require a retest. Certain factors, like topical corticosteroids or food and drink residues, can also interfere with the results. While functional medicine practitioners often use salivary cortisol testing to assess HPA axis imbalances, conventional endocrinologists mainly rely on it for diagnosing conditions like Cushing’s syndrome or Addison’s disease, rather than subtler issues like adrenal fatigue. Understanding both the advantages and limitations of this method helps clinicians choose the right diagnostic tools. While salivary testing provides valuable insights, it’s often most effective when combined with other approaches to assess adrenal function comprehensively.
Blood and Serum Hormone Testing
Key Hormones Measured
Blood tests are a common method for evaluating adrenal function by analyzing hormone levels during their peak times. For example, morning cortisol – typically measured between 6:00 AM and 9:00 AM – helps determine adrenal health. A cortisol level of 18 mcg/dL or higher generally excludes adrenal insufficiency, while levels 3 mcg/dL or lower strongly indicate it. These tests usually measure total cortisol, which includes both the bound and free hormone fractions.
When cortisol levels are low, the accompanying ACTH levels can help pinpoint the issue. High ACTH with low cortisol points to primary adrenal insufficiency, whereas low or normal ACTH suggests a pituitary-related problem. Low DHEA-S levels can further clarify cases where cortisol levels are ambiguous. Additionally, TSH is often tested since thyroid disorders can mimic adrenal dysfunction with symptoms like fatigue and weight changes. Some hormone panels also include aldosterone and renin, which assess the adrenal glands’ role in regulating salt and water balance. This function is typically impaired in primary adrenal insufficiency but remains intact in secondary cases.
While these measurements are essential, they must be viewed with an understanding of the limitations inherent to blood testing.
Limitations of Blood Tests
Blood tests, though useful, have several drawbacks. Cortisol secretion occurs in 8–10 pulses per day, meaning a single blood sample only provides a snapshot of hormone levels at that moment. Additionally, the stress of a blood draw can temporarily raise cortisol levels, potentially concealing an underlying deficiency.
Other factors can complicate interpretation. For instance, oral contraceptives and pregnancy increase corticosteroid-binding globulin (CBG), which can falsely elevate total cortisol readings even when the biologically active free cortisol is low. Similarly, high-dose biotin supplements (over 5 mg/day) may interfere with immunoassays, leading to inaccurate results. Modern LC-MS/MS assays – considered more precise – often yield cortisol readings that are 25–30% lower than older methods, requiring adjusted reference thresholds.
Although blood tests are a valuable starting point for assessing adrenal function, they may not fully capture the dynamic and fluctuating nature of hormone activity. This highlights the need for careful interpretation and, in some cases, additional testing methods to gain a clearer picture.
How To Accurately Test & End Adrenal Fatigue + Dr. Maggie’s Fight or Flight Story
sbb-itb-d9e542d
Urine Testing for Adrenal Function
Urine testing plays a key role in evaluating adrenal function by measuring cortisol levels and their metabolites. Similar to salivary and blood tests, it provides valuable insights, but with additional details on how cortisol is metabolized. The 24-hour urinary free cortisol (UFC) test is a standard approach, capturing all unbound cortisol filtered by the kidneys over a full day. Normal ranges typically fall below 45 mcg/24 hours for women and 60 mcg/24 hours for men. To perform this test, all urine is collected in a large container for 24 hours, starting after the first morning void. The sample must be refrigerated during the collection period, and patients are advised to avoid intense physical activity the day before, as it could artificially elevate cortisol levels.
Multi-Point Dried Urine Testing
Dried urine testing builds upon the 24-hour UFC test by offering a more detailed analysis of adrenal function. This modern method uses dried urine filter strips, collected at four specific times throughout the day – usually around 8:00 AM, noon, 4:00 PM, and midnight. By mapping daily cortisol patterns and its inactive metabolite, cortisone, this test provides insight into the rates of hormone metabolism. Unlike blood or saliva tests that focus solely on parent hormones, dried urine testing evaluates up to 44 unique markers, including 13 estrogens, 8 androgens, and various glucocorticoid metabolites. This level of detail is particularly helpful for patients with normal salivary cortisol levels who still exhibit symptoms of adrenal dysfunction. It reveals whether cortisol is being metabolized too quickly or too slowly. Additionally, the stability of the dried strips for up to 30 days makes mailing samples to labs more convenient. This method provides a deeper look at adrenal health compared to saliva testing.
Comparison to Saliva Testing
Both saliva and dried urine testing capture cortisol’s diurnal rhythms, but they differ in what they measure. Saliva testing focuses on free (bioavailable) cortisol, which represents the actively circulating hormone in the body. Dried urine testing, on the other hand, measures both free cortisol and its metabolites, shedding light on both hormone production and how the body clears it. This makes urine testing especially useful for individuals who struggle with saliva collection or cannot produce enough saliva. While saliva testing excels at mapping cortisol’s "stress curve" throughout the day, dried urine testing offers a broader view of how cortisol is processed after being produced.
| Test Method | Collection Approach | What It Measures | Best For |
|---|---|---|---|
| 24-Hour UFC | All-day liquid collection | Total daily free cortisol | Screening for Cushing’s or Addison’s disease |
| Multi-Point Dried Urine | 4 filter strips at specific times | Free cortisol, cortisone, and 44+ metabolites | Evaluating hormone rhythm and clearance |
| Saliva Testing | Swab or tube at multiple times | Free cortisol at specific moments | Mapping bioavailable hormone patterns |
Interpreting Test Results and Clinical Correlation
Common Patterns in Adrenal Fatigue
After conducting thorough testing, clinicians analyze results to uncover typical adrenal dysfunction patterns. Normally, cortisol levels peak around 8:00 AM and gradually decline, reaching their lowest point by 10:00 PM. When this rhythm is disrupted, it may signal adrenal issues. A frequently observed pattern is the 2:00–3:00 PM energy crash, where cortisol levels drop too low in the afternoon, leaving individuals feeling drained and often craving caffeine or sugary snacks. Another common issue is the "wired but tired" phenomenon, where cortisol levels stay elevated at night, making it hard to fall asleep despite feeling utterly fatigued.
Practitioners often focus on a "grey zone" in morning cortisol levels, typically between 5.4–10.8 mcg/dL (150–300 nmol/L). While technically within the normal range, this level often aligns with symptoms like extreme fatigue, cravings for salty foods, and difficulty managing stress. On the other hand, true adrenal insufficiency, such as Addison’s disease, is characterized by cortisol levels below 3 mcg/dL, often accompanied by noticeable symptoms like electrolyte imbalances and skin darkening. The distinction lies in severity – adrenal fatigue reflects reduced adrenal function, while Addison’s represents near-total failure of the adrenal glands.
Integrating Symptoms with Test Results
Interpreting test results effectively requires pairing lab data with the patient’s symptoms.
"The diagnosis of adrenal insufficiency requires a critical level of clinical suspicion." – UpToDate
Lab results alone rarely tell the full story. For instance, a patient with an 8:00 AM cortisol level of 6.5 mcg/dL may fall within the "normal" range of 4–22 mcg/dL but still experience significant symptoms that warrant further investigation. This is why practitioners pay close attention to patterns such as reliance on coffee, cravings for carbohydrates, or experiencing a "second wind" around 9:00–10:00 PM. These observations help connect symptoms with lab findings.
Additionally, a detailed medical history can uncover factors that might skew results. For example, patients taking oral estrogen may show artificially elevated cortisol levels due to increased cortisol-binding globulin (CBG). Likewise, individuals with disrupted circadian rhythms – such as shift workers or frequent travelers – may have unreliable single-point cortisol readings. Combining symptom tracking with well-timed testing allows practitioners to distinguish true adrenal dysfunction from misleading test artifacts. This holistic approach helps guide tailored treatment plans in line with functional medicine principles.
Table: Normal vs. Abnormal Test Patterns
| Test Type | Normal/Optimal Range (8 AM) | Suboptimal/Abnormal Finding | Clinical Correlation |
|---|---|---|---|
| Serum Cortisol | 11–18 mcg/dL | <3 mcg/dL | Severe fatigue, weight loss, low blood pressure |
| Serum Cortisol | 11–18 mcg/dL | 4–10 mcg/dL (Low Normal) | Afternoon energy crash, caffeine dependency |
| Serum Cortisol | 11–18 mcg/dL | >20 mcg/dL (High Normal) | Anxiety, insomnia, "wired" sensation |
| Salivary Cortisol | >5.9 nmol/L | <1.0 nmol/L | Suggests primary adrenal failure |
| Urine (DUTCH) | Smooth diurnal curve | Spikes at night or flat curve | "Second wind" at 10 PM or chronic exhaustion |
At Kinnection Clinic, clinicians combine these diagnostic insights with detailed symptom profiles to create personalized strategies aimed at improving adrenal function and overall well-being.
Conclusion
The Role of Testing in Effective Treatment
Thorough testing does more than confirm a diagnosis – it safeguards against potentially harmful errors. Without proper lab work, conditions like hypothyroidism or clinical depression can be mistaken for adrenal fatigue, leading to ineffective or even harmful treatments. For instance, the misuse of adrenal supplements can have serious consequences. As the Endocrine Society cautions:
"If you take adrenal hormone supplements when you don’t need them, your adrenal glands may stop working and become unable to make the hormones you need when you are under physical stress."
This kind of misuse can result in a dangerous adrenal crisis during times of stress. Accurate testing methods – such as 9:00 AM serum cortisol tests, salivary mapping, or dried urine analysis – are essential for distinguishing between true adrenal insufficiency (like Addison’s disease) and stress-related patterns. Clinical decision-making often relies on sensitivity and specificity thresholds (commonly 0.9 and 0.7, respectively). For borderline results, clinical expertise is key to crafting targeted interventions. These might include dietary changes, stress reduction techniques, and nutritional support, all aimed at addressing the root causes effectively. Reliable diagnostic data forms the backbone of a well-rounded treatment approach.
Moving Forward with Functional Medicine
Once a clear diagnosis is established, functional medicine provides a pathway for comprehensive care. This approach goes beyond simply prescribing hormone replacements by examining interconnected systems like gut health, thyroid function, and blood sugar regulation. Using tools like detailed cortisol mapping and nutrient evaluations, practitioners create personalized treatment plans. These plans might include strategies such as targeted B vitamin supplementation, adaptogens, improved sleep routines, and metabolic support. The ultimate aim isn’t just to normalize cortisol levels but to help the body regain its natural resilience and energy.
At Kinnection Clinic, this systems-based perspective is paired with individualized wellness plans. By addressing root causes through functional medicine – and incorporating hormone replacement therapy when necessary – the clinic empowers patients to move beyond fatigue and toward lasting vitality. Whether it’s improving sleep hygiene, integrating gentle exercise like yoga or walking, or stabilizing blood sugar with protein-rich and complex carbohydrate meals, the focus is always on sustainable, long-term healing tailored to each patient’s needs.
FAQs
How is adrenal fatigue different from adrenal insufficiency?
Adrenal fatigue and adrenal insufficiency are two terms that often get mixed up, but they refer to very different things. Adrenal fatigue is a term commonly used by some integrative health practitioners to describe symptoms such as persistent tiredness, difficulty handling stress, anxiety, and sleep disturbances. These symptoms are thought to stem from overworked adrenal glands due to prolonged stress. However, it’s important to note that adrenal fatigue is not an officially recognized medical condition, and there aren’t any scientifically validated tests to confirm its existence.
In contrast, adrenal insufficiency is a medically acknowledged condition. It occurs when the adrenal glands don’t produce enough cortisol, and in some cases, aldosterone. This condition can result from autoimmune disorders, infections, surgical procedures, or issues with the pituitary gland. Diagnosis involves specific hormone tests, like measuring morning cortisol levels or using ACTH stimulation tests, to verify insufficient cortisol production.
If you’re dealing with symptoms that might be linked to adrenal fatigue, Kinnection Clinic offers functional medicine evaluations. They can help address your concerns and conduct the necessary hormone tests to rule out adrenal insufficiency.
What’s the difference between salivary, blood, and urine cortisol tests for assessing adrenal function?
Salivary cortisol tests offer a simple, stress-free way to monitor free cortisol levels throughout the day. These tests are particularly useful because they capture your body’s natural daily rhythm. Unlike blood tests – which measure total cortisol and can be skewed by stress during collection or fluctuations in cortisol-binding proteins – salivary tests provide a clearer picture of adrenal function without the added anxiety of a needle.
Urine tests, by contrast, measure the total cortisol your body excretes over a 24-hour period. While they’re helpful for gauging overall cortisol production, they don’t reveal the daily fluctuations that salivary tests can pick up. What makes salivary testing stand out is its ease of use, accuracy, and its ability to offer real-time insights into your adrenal activity as you go about your day.
Can lifestyle changes help alleviate symptoms of adrenal fatigue?
Yes, making specific lifestyle changes can go a long way in easing symptoms like fatigue, brain fog, and mood swings often tied to adrenal dysfunction. Managing chronic stress is a key part of this. Practices such as mindfulness, gentle physical activity, and prioritizing high-quality sleep can help regulate cortisol levels, which are crucial for keeping energy steady throughout the day.
What you eat matters, too. Emphasizing whole, nutrient-rich foods, keeping carbohydrate intake consistent, and cutting back on caffeine and alcohol can help stabilize blood sugar levels and avoid those dreaded energy dips.
Clinics like Kinnection Clinic offer personalized testing, such as saliva cortisol assessments, to pinpoint imbalances. This allows for customized plans that might include stress management strategies, tailored nutritional advice, and, when needed, supplements or chiropractic care to support overall health. While "adrenal fatigue" isn’t officially recognized as a medical diagnosis, many people find that these holistic methods improve their energy, sleep, and ability to handle stress.



