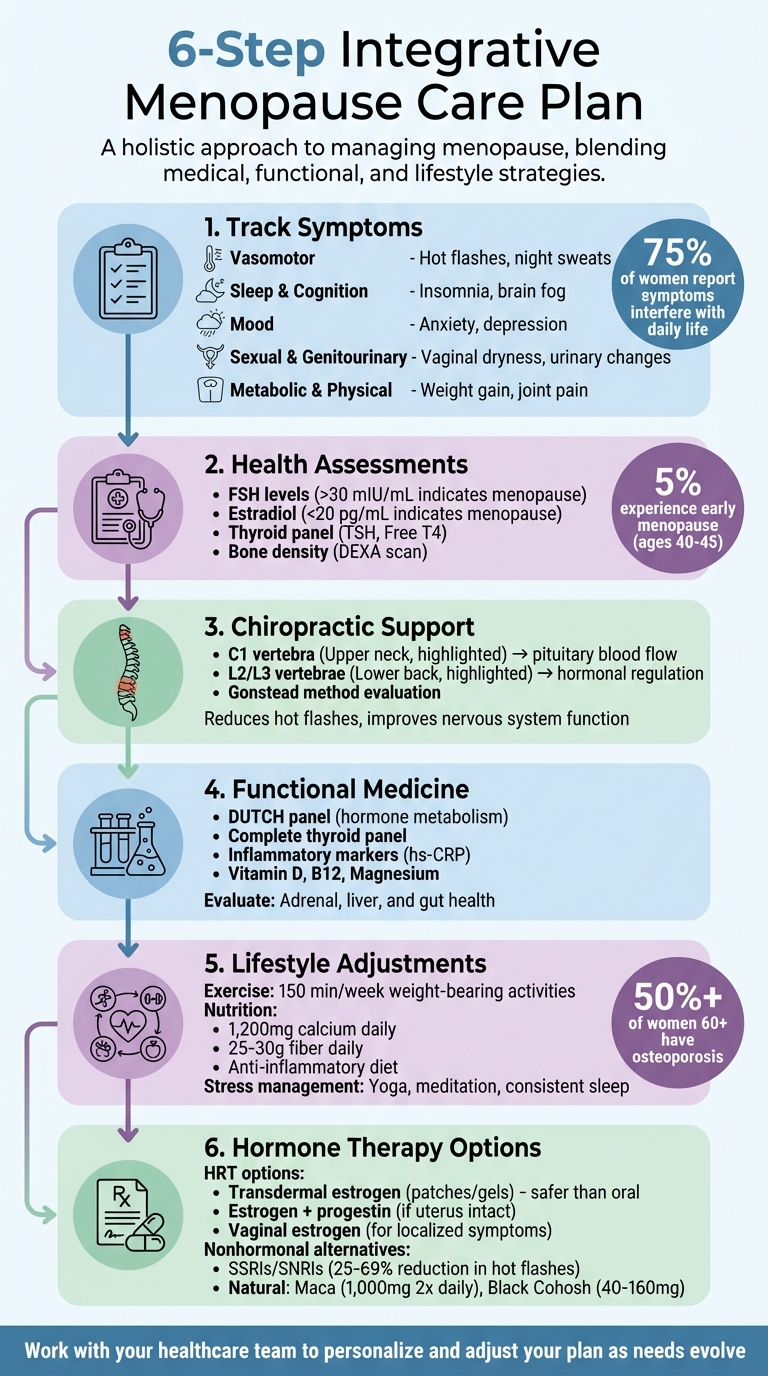
Managing menopause can feel overwhelming, but an integrative approach simplifies the process. Combining traditional treatments like hormone therapy with complementary strategies – such as chiropractic care, functional medicine, and lifestyle changes – can help address symptoms like hot flashes, sleep issues, and mood swings. Here’s how to create a personalized menopause care plan:
- Track Symptoms: Monitor issues like hot flashes, sleep disturbances, and mood changes by category to identify patterns.
- Health Assessments: Understand your menopause stage, review your medical history, and use lab tests (e.g., FSH, estradiol) to confirm hormonal changes.
- Chiropractic Support: Address spinal alignment to reduce symptoms like hot flashes and improve nervous system function.
- Functional Medicine: Dive deeper into hormone balance by evaluating adrenal, liver, and gut health with advanced tests like the DUTCH panel.
- Lifestyle Adjustments: Focus on weight-bearing exercises, anti-inflammatory diets, and stress management to support bone health, energy, and overall well-being.
- Hormone Therapy Options: Consider HRT or nonhormonal alternatives tailored to your needs, risks, and preferences.
This guide emphasizes tracking, testing, and tailoring strategies for your unique experience. Start with lifestyle changes, incorporate targeted treatments, and work closely with healthcare providers to refine your plan. Menopause care isn’t one-size-fits-all – your approach should reflect your symptoms, goals, and evolving needs.
6-Step Integrative Menopause Care Plan Checklist
How to Navigate Menopause & Perimenopause for Maximum Health & Vitality | Dr. Mary Claire Haver
Symptom and History Assessment
Before creating a menopause care plan, it’s important to identify your transition stage and understand the changes happening in your body. This step helps you and your healthcare team determine the best options tailored to your needs. Start by pinpointing your menopausal stage and reviewing your health history to build a strong foundation for your personalized care.
Determine Your Menopause Stage and Review Medical History
The first step is figuring out your menopause stage. Perimenopause, which can last 4–8 years, is marked by fluctuating hormone levels that cause symptoms like irregular periods, hot flashes, and mood swings. Menopause itself begins after 12 consecutive months without a period, typically around age 51. Postmenopause follows, a phase where hormone levels stabilize but the risks for conditions like osteoporosis and heart disease increase.
For some, menopause happens earlier. About 5% of women experience early menopause between ages 40 and 45, and 1% face premature menopause before age 40. Women who’ve had a hysterectomy may need lab tests, such as FSH and estradiol levels, to confirm their menopausal status.
"Menopause is identified clinically, meaning that it can be recognized based on the patient’s age and history." – Dr. Jaime Cloyd, ND
It’s also crucial to document your medical history, including surgeries, family health conditions (like heart disease, osteoporosis, or thyroid disorders), and metabolic concerns such as PCOS. This information helps determine if hormone replacement therapy is suitable and distinguishes menopause-related symptoms from other potential health issues.
Track Symptoms by Body System
Roughly 75% of individuals going through menopause report that their symptoms interfere with daily life. To better manage these challenges, track your most bothersome symptoms across these categories:
- Vasomotor: Hot flashes, night sweats, and chills
- Menstrual: Irregular periods and missed cycles
- Sleep and Cognition: Insomnia, sleep disturbances, brain fog, and memory lapses
- Mood: Anxiety, irritability, depression, and lack of motivation
- Sexual and Genitourinary: Vaginal dryness, painful intercourse, low libido, and urinary urgency or frequency
- Metabolic and Physical: Sudden weight gain (especially around the abdomen), thinning hair, dry skin or eyes, and breast tenderness
Digital tools, like the Ovia app, can make it easier to track these symptoms and share the data with healthcare providers who specialize in menopause care.
Monitor Health Metrics and Lab Tests
Keeping an eye on key health metrics – such as blood pressure, weight, and waist circumference – offers valuable data to complement your symptom tracking. Women over 65, or those with specific risk factors, should also consider bone density testing (DEXA) to evaluate their risk for osteoporosis.
When it comes to lab work, certain results can confirm menopause. FSH levels consistently above 30 mIU/mL, paired with estradiol levels below 20 pg/mL, usually indicate menopause. However, a well-rounded evaluation goes beyond just sex hormones. Annual tests should include a thyroid panel (TSH and Free T4) to rule out thyroid issues, which can mimic menopause symptoms. Additional labs, like a Comprehensive Metabolic Panel (CMP), Hemoglobin A1c, and Lipid Panel, can help assess cardiovascular and metabolic health. Testing for Vitamin D, B12, and other micronutrients is also helpful for supporting bone and nerve health.
For accurate hormone testing during menstruation, schedule blood work on Day 3 of your cycle and stop taking biotin 72 hours before testing. If you’re looking for a convenient option, the Labcorp OnDemand Menopause Test measures four key hormones and costs $139. These results can guide further evaluations, including spinal health assessments and integrative care strategies.
Chiropractic and Spinal Health Checklist
Your spine plays a crucial role in managing menopause symptoms. Misalignments in the spine can interfere with the communication between your brain and endocrine glands, including the hypothalamus. This disruption can lead to common menopausal challenges like hot flashes, mood swings, and sleep problems. By focusing on spinal health through Gonstead chiropractic care, you can reduce inflammation, improve blood circulation, and support proper nervous system function during this transitional phase.
Check Your Posture and Alignment
Take a moment to stand in front of a mirror. Check if your ears, shoulders, and hips are in a straight line. Look for signs like a forward head position, uneven hips, or an unsteady gait. These could indicate underlying issues such as pelvic, knee, or foot dysfunction. Spotting these visual cues early can help identify areas where chiropractic adjustments may be beneficial.
Gonstead Chiropractic Evaluation and Progress Tracking
Gonstead chiropractic care uses a detailed approach to identify and address spinal misalignments. This includes methods like visualization, palpation, instrumentation, X-rays, and symptom analysis. Tools such as the Nervoscope – a dual-probe instrument – help detect temperature differences along the spine, which can signal nerve irritation.
"Nonsurgical spine care works best when the plan fits the person – their job, their stressors, their movement habits – and when the clinician and patient stay in dialogue about what’s working." – Dr. Alexander Jimenez, DC, APRN, FNP-BC
Tracking your progress is key. Improvements in areas like pain relief, energy levels, sleep quality, and mobility are common. Many patients also report relief from non-musculoskeletal symptoms, such as hot flashes, night sweats, and better bladder control, following spinal adjustments. Targeting specific vertebrae, like C1 (linked to blood flow to the pituitary gland) and L2/L3 (connected to hormonal regulation), can enhance nervous system function and support hormonal balance during menopause. These adjustments work well alongside functional medicine approaches for a more comprehensive strategy.
Kinnection Clinic‘s Chiropractic Services
At Kinnection Clinic, Gonstead chiropractic care is tailored to fit into a holistic menopause wellness plan. Using advanced diagnostic tools like digital X-rays and specialized Gonstead instruments, the clinic creates personalized adjustment strategies to address the root causes of spinal dysfunction. Paired with functional lifestyle recommendations, their services integrate chiropractic care with hormone replacement therapy, nutritional guidance, and other functional medicine practices, offering well-rounded support for menopausal health.
Functional Medicine and Hormone Balance Checklist
Menopause brings about a whirlwind of metabolic changes, impacting everything from insulin sensitivity to bone health, cardiovascular function, and even neurological well-being. Functional medicine takes a deeper dive than standard care, focusing on how your body produces, processes, and eliminates hormones. This involves assessing the adrenal glands (which step in to produce hormones as ovarian function declines), the liver (responsible for breaking down hormones), and the gut microbiome – particularly the estrobolome, which plays a key role in estrogen metabolism.
"Menopause isn’t simply about estrogen deficiency but involves complex changes in insulin sensitivity, bone metabolism, cardiovascular function, and neurological health that require comprehensive evaluation and treatment." – Dr. Kristi Vaughan, DC, BCN, BCIA, BSBA, Vaughan Vitality Wellness
To get a full picture of your hormonal health, targeted lab testing is essential.
Complete Root Cause and Lab Evaluations
Routine tests often miss the bigger picture, but more detailed evaluations can uncover the root causes of hormonal imbalances. Start with the DUTCH (Dried Urine Test for Comprehensive Hormones) panel, which not only measures hormone levels but also evaluates how your body metabolizes them and tracks your daily cortisol rhythm. A complete thyroid panel (including TSH, Free T3, Free T4, Reverse T3, and thyroid antibodies) is crucial, as thyroid dysfunction can mimic or exacerbate menopausal symptoms.
To assess metabolic health, include Hemoglobin A1c, fasting insulin, and a full lipid panel (with Lipoprotein(a)), as cardiovascular risks rise post-menopause. Inflammatory markers like high-sensitivity C-reactive protein (hs-CRP) and nutrient levels (Vitamin D, B vitamins, Magnesium) should also be checked. For baseline FSH, LH, and Estradiol levels, timing your tests correctly within your cycle is important.
Review Hormone Therapy and Nonhormonal Options
Hormone replacement therapy (HRT) is the go-to solution for managing hot flashes and night sweats, but it’s not the only option. For women under 60 or within a decade of menopause, the benefits of HRT often outweigh the risks. If you still have your uterus, a combination of estrogen and progestin is needed to prevent endometrial cancer. Transdermal estrogen (like patches or gels) is a safer choice than oral forms, as it carries a lower risk of blood clots and stroke. For vaginal dryness or atrophy, localized vaginal estrogen is highly effective and has minimal systemic absorption.
If HRT isn’t an option – due to a history of breast cancer or blood clots, for example – nonhormonal treatments like SSRIs, SNRIs, or gabapentin can reduce hot flashes by 25% to 69%. Natural remedies such as phytoestrogens (found in soy and flaxseed), Maca (1,000 mg twice daily), Black Cohosh (40–160 mg), and Red Clover (40–80 mg isoflavones) are also worth considering. At Kinnection Clinic, functional medicine consultations include advanced testing and personalized hormone optimization plans, often incorporating bioidentical hormone therapy tailored to your unique needs.
Implement Functional Lifestyle Strategies
Daily habits play a key role in supporting your hormone health and complementing lab evaluations or therapies. Start with an anti-inflammatory diet packed with cruciferous vegetables to aid liver detoxification. Make sure to consume 25–30 grams of fiber daily to promote regular bowel movements, which help eliminate hormone metabolites. Adequate protein intake is also essential for maintaining muscle mass and supporting metabolic health.
For liver support, consider Milk Thistle (150–300 mg silymarin, 2–3 times daily) or N-Acetyl Cysteine (600–1,200 mg daily). If stress is causing symptom flare-ups, adaptogens like Ashwagandha (250–1,000 mg) or Rhodiola (100–600 mg) can help regulate your adrenal response. For vaginal dryness, 100 IU of Vitamin E used vaginally has been shown to be as effective as estrogen. Additionally, using a Continuous Glucose Monitor (CGM) can help you track blood sugar spikes that may be affecting your hormone balance.
sbb-itb-d9e542d
Lifestyle and Nervous System Regulation
Your daily habits play a big role in how your body responds to the drop in estrogen levels. As cortisol levels rise, symptoms like fatigue, anxiety, weight gain, insomnia, and brain fog can become more pronounced. Making intentional lifestyle changes can help regulate your nervous system and ease these symptoms. These adjustments also set the stage for physical activities that support stronger bones and muscles.
Exercise for Bone and Muscle Health
Bone loss speeds up significantly during the first 3–6 years of menopause, with over half of women aged 60 and older experiencing osteoporosis. Incorporating weight-bearing exercises – like running, brisk walking, jumping, or dancing – can stimulate bone-forming cells, encouraging new tissue growth and even increasing bone diameter. Aim for 150 minutes of these activities each week to help maintain bone density.
"Weight-bearing exercises are crucial to help prevent osteoporosis and improve bone health." – Tina Zhang, MD, Assistant Professor of Medicine, Johns Hopkins University School of Medicine
Strength training is just as essential. Performing resistance exercises 2–3 times a week using weights, bands, or even your own body weight can help combat the natural muscle loss that occurs during menopause. Moves like pushups, squats, planks, and lunges target your core and limbs. To improve balance and reduce the risk of falls – a leading cause of fractures in postmenopausal women – try practices like Tai Chi or Yoga on most days. While swimming and cycling are great for cardiovascular fitness, they don’t provide the same bone-strengthening benefits as weight-bearing activities.
Improve Sleep and Manage Stress
As estrogen levels drop, your body’s ability to manage stress can falter, leading to sleep problems and heightened anxiety. Practices like mindfulness meditation and yoga can help by lowering cortisol levels and improving overall well-being. Research from 2018, which reviewed 13 studies involving more than 1,300 participants, found that yoga significantly alleviated both physical and psychological symptoms of menopause.
Stick to a consistent sleep routine and minimize exposure to screens, caffeine, and alcohol before bedtime. Daily mindfulness meditation can also help regulate cortisol. Social connections matter too – nurturing relationships and engaging in physical touch, like hugging, can actively lower stress hormones. Limit alcohol to no more than 14 units per week (around 2 units per day) and cut back on caffeine, as both can worsen sleep issues and stress during menopause. Pairing these strategies with proper nutrition can further support hormonal balance.
Optimize Nutrition and Hydration
What you eat directly impacts hormonal balance. Stabilizing blood sugar is key – pair unrefined, low-sugar carbs (like whole grain bread, rice, or pasta) with proteins and healthy fats to avoid energy crashes and reduce anxiety. Filling half your plate with fruits and vegetables at every meal can help ease hot flashes and improve sleep quality. In fact, postmenopausal women who consume 4.7 grams of whole grain fiber per 2,000 calories lower their risk of premature death by 17%.
"A woman needs to support these changes during menopause just as she would in pregnancy – by adjusting her eating habits and focusing on her overall health." – Monilla Dent, M.D., OB/GYN
Calcium needs increase during menopause, jumping from 700mg to 1,200mg daily to help maintain bone density. Include calcium-rich foods like dairy, fortified plant milks, and canned fish in your diet. During fall and winter, supplement with 10mcg (400IU) of vitamin D to aid calcium absorption. Swap saturated fats for unsaturated options like olive oil, avocados, seeds, and nuts to support heart health. To prevent muscle loss, include quality protein in every meal – think beans, salmon, eggs, or Greek yogurt. Stay hydrated with water and herbal teas such as green or black tea, which naturally contain phytoestrogens. Finally, try to limit or avoid common hot flash triggers like caffeine, alcohol, spicy foods, and processed items high in salt.
Create Your Personalized Action Plan
Using your symptom and lab evaluations as a foundation, craft a care plan tailored to your priorities. This plan should be flexible enough to adapt as your needs shift over time.
Set Goals and Prioritize Strategies
Start by identifying your most bothersome symptoms and ranking them by urgency. Then, decide whether to focus on lifestyle adjustments or hormone therapy based on your menopausal stage, which can be confirmed through FSH and estradiol levels.
"The tool can help you sort out the best options, given your preferences. Do you want to take medications or avoid them? … Do you want to avoid treatments that are riskier? Personalize your options." – MyMenoPlan
Build a layered approach to your care plan. Begin with foundational lifestyle changes, such as adopting a Mediterranean diet and incorporating weight-bearing exercises. If needed, add targeted supplements like Maca (1,000 mg twice daily) or Black Cohosh to address specific symptoms like hot flashes. If these steps aren’t enough, consider adjusting your treatment approach. Be mindful of potential barriers, such as time, cost, or access to specialists, and plan ways to overcome them.
Coordinate Care with Your Healthcare Team
Create a list of all your healthcare providers, including your primary care physician, nutritionist, chiropractor, and hormone consultant, and clarify their roles in your care. Continue with routine health screenings, such as annual physicals, mammograms, and colonoscopies. Initially, schedule follow-up appointments every 30–60 days to monitor how well your treatment plan is working. If you’re seeing an out-of-network specialist, ask for a "Superbill" with billing codes like 99204 or 99214 to seek potential insurance reimbursement.
"Compassionate, Respectful Care where you feel seen, heard, and empowered – you are in the drivers seat at all times here." – Dr. Erin Thorne, ND, IFMCP
Make sure your annual checkups include cardiometabolic and thyroid function labs, such as Hemoglobin A1c and lipid panels, as menopause can raise the risk of heart and thyroid conditions. If you’re over 65 or have risk factors for osteoporosis, schedule a bone density test (DEXA scan). To make the most of your appointments, bring a symptom log tracking things like hot flash frequency, sleep quality, and mood changes. Regular updates will help fine-tune your plan.
Track Progress and Adjust Your Plan
Revisit your plan monthly to evaluate whether symptoms are improving or persisting. Compare your current symptoms to your baseline and note any side effects from treatments. If a particular strategy isn’t effective after 60–90 days, discuss alternative options with your provider. Your treatment plan should evolve as your needs change.
Celebrate small achievements, such as consistently incorporating weight-bearing exercises or making other lifestyle improvements. Keep refining your plan as you move through different stages of menopause – what works during perimenopause might need adjustments in postmenopause. Stay flexible and open to changes as you continue on your journey.
Conclusion
This checklist pulls together the essential steps to help you create a menopause care plan tailored to your needs. With up to 70% of women experiencing symptoms that can disrupt daily life, addressing these challenges requires more than a one-size-fits-all solution. An integrative approach looks at the bigger picture, tackling symptoms from multiple angles and focusing on the root causes of hormonal imbalances.
Creating a personalized care plan means working closely with your healthcare team. Begin with foundational lifestyle changes – like incorporating weight-bearing exercises, following an anti-inflammatory diet, and managing stress. From there, add targeted interventions such as hormone therapy or chiropractic care based on your symptom tracking and lab results. This layered strategy not only helps alleviate immediate discomfort but also lowers long-term health risks.
At Kinnection Clinic, services like Gonstead chiropractic care, functional medicine, and customized hormone therapies are designed to embrace this integrative approach. Their team crafts personalized wellness plans that adapt to your evolving needs during menopause, addressing the underlying causes of your symptoms. Whether you’re navigating the early stages of perimenopause or focusing on postmenopausal health, professional guidance ensures your plan is both effective and safe.
Think of this checklist as your guide to blending lifestyle changes with expert care. Keep track of your progress, celebrate small victories, and adjust your strategies as your body transitions. With the right mix of self-care and professional support, you can face menopause with confidence and energy.
FAQs
How can I identify my menopause stage, and why does it matter?
Determining where you are in the menopause journey starts with tracking your menstrual history and recognizing symptoms. Perimenopause often begins when your periods become irregular, accompanied by signs like hot flashes, night sweats, mood swings, or sleep disturbances. Menopause, on the other hand, is officially confirmed after you’ve gone 12 months in a row without a period. While hormone tests, such as follicle-stimulating hormone (FSH) levels, can sometimes help pinpoint your stage, they’re not always required.
Understanding your stage matters because each phase comes with its own set of health priorities. During perimenopause, the focus is on managing symptoms through lifestyle changes, proper nutrition, or short-term treatments. Once menopause is reached, care shifts toward long-term goals like preserving bone density, promoting heart health, and addressing lingering symptoms. At Kinnection Clinic, we take an integrative approach, combining Gonstead chiropractic care and functional medicine to evaluate your stage and develop a personalized plan for your ongoing well-being.
How can chiropractic care help manage menopause symptoms?
Chiropractic care can be an effective way to manage menopause symptoms by focusing on spinal alignment and nervous system health, both of which may be affected during this hormonal shift. Through gentle and precise spinal adjustments, chiropractic treatment can help ease back and joint pain, enhance nerve communication, and contribute to improved sleep, reduced stress, and better hormonal balance.
At Kinnection Clinic, the Gonstead chiropractic method is combined with functional medicine, hormone replacement therapy, and IV nutrition to offer a tailored care plan. This integrated approach aims to address common menopause challenges like hot flashes, disrupted sleep, and fatigue, while also supporting overall energy and well-being.
What are some effective nonhormonal ways to manage menopause symptoms?
There are various ways to manage menopause symptoms without relying on hormones. Options include cognitive-behavioral therapy (CBT), clinical hypnosis, and medications like SSRIs, SNRIs, or gabapentin. For more targeted relief, treatments such as the neurokinin-3 antagonist fezolinetant or oxybutynin may also be effective.
Making changes to your daily routine can also have a positive impact. Practices like yoga, acupuncture, and mindfulness meditation can enhance overall well-being. Other mind-body techniques may also be worth exploring. Maintaining a healthy weight is another important step. For those seeking advanced treatments, a stellate ganglion block might be an option. Always consult with a healthcare provider to develop a care plan that works best for you.



